
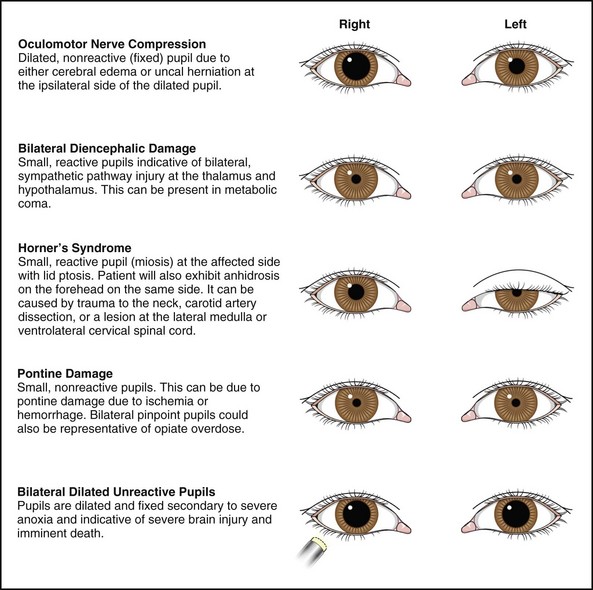
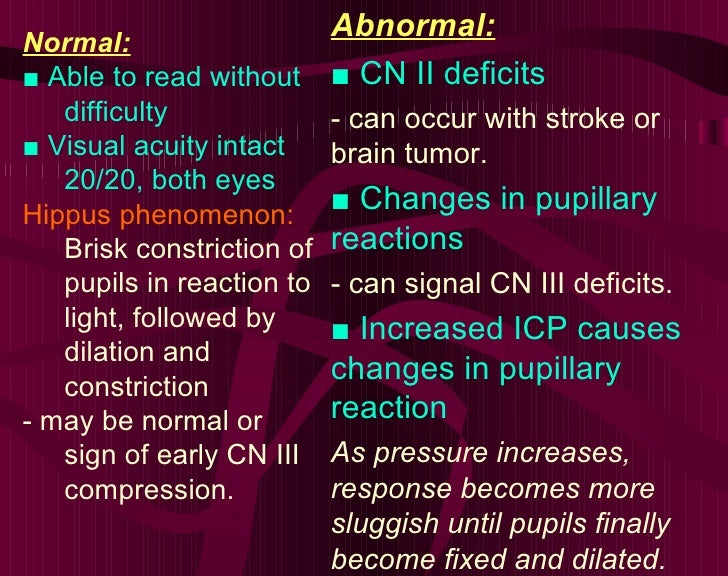
Third nerve palsy results from damage to the oculomotor nerve anywhere along its route from the nucleus in the dorsal mesencephalon, its fascicles in the brainstem parenchyma, the nerve root in subarachnoid space, the cavernous sinus or the posterior orbit. 3,6,7,11 Occasionally, head trauma is associated with the development of CN III palsy. 7 Often, there is concurrent diabetes and/or hypertension in older adults. CN III palsy is uncommon in children, although it can occur. Patients who develop acute CN III palsy tend to be older (>55 years of age). Various neurological signs-such as contralateral intention tremor, cerebellar ataxia or contralateral hemiplegia-may present concomitantly with the development of CN III palsy, depending on the cause and location of damage to CN III within the brainstem. 5-7 In any case of CN III palsy, the pupil may be dilated and minimally reactive to light (pupillary involvement), totally reactive and normal (pupillary non-involvement) or sluggishly responsive (partial pupillary involvement).
1-3 The underaction of these muscles may be complete or incomplete. There is limitation of elevation, depression and adduction as well as an underaction of the superior, inferior and medial recti muscles and the inferior oblique muscle. Acuity typically is unaffected unless the provoking lesion occurs in the superior orbital fissure, causing simultaneous CN II involvement.ĬN III palsy produces a non-comitant exotropic, hypotropic eye position (down and out). But, in some instances, the diplopia may be masked by the ptosis, which obscures the vision in the affected eye however, when the lid is manually elevated, the patient will experience diplopia. 1-4 Such patients often complain of double vision.


In left gaze, he demonstrates an inability to adduct anisocoria also is evident.Ī patient with acute CN III palsy usually presents with a sudden onset of unilateral ptosis and ophthalmoplegia, which is frequently accompanied by significant eye or head pain––depending on the underlying cause. Our patient in primary gaze with right ptosis and an eye that appears down and out (top). In this month’s column, we discuss one of the only true ophthalmic emergencies: aneurysmal CN III palsy. The dilated right pupil and severe hemicranial pain indicated that the likely cause was an intracranial aneurysm, which was compressing the nerve and pupillomotor fibers. Tellingly, his right pupil was mid-dilated and minimally reactive to light, while the left pupil was smaller and normally reactive.Ĭlearly, the patient had a right CN III palsy.
Abduction was normal in the right eye and motility was normal in the left. He had significant ophthalmoplegia with an adduction, elevation and depression deficit. Upon manually elevating the lid, the right eye had assumed a “down-and-out” position. He took over-the-counter analgesics throughout the weekend and, when the debilitating pain did not subside, he came into the office urgently on Monday morning.Įvaluation revealed a well-nourished man in acute distress with a near complete right-sided ptosis. The patient is a 61-year-old black male being managed for POAG who developed a severe headache on a Friday, which he described as “right sided” and a “nine out of 10” in terms of pain and discomfort severity.Īt nearly the same time as the onset of his headache, his right eyelid began to droop and he developed double vision. This month, we discuss yet another patient with glaucoma who developed double vision from a more sinister cause. Double Trouble,” we described a patient who was being managed for primary open-angle glaucoma (POAG) and subsequently developed double vision from coincident cranial nerve (CN) VI palsy.


 0 kommentar(er)
0 kommentar(er)
